
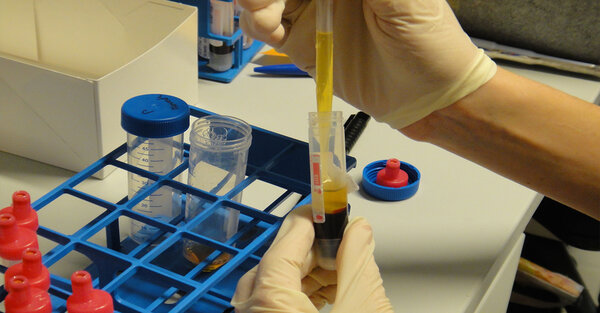
Since many years, the clinical department of Neurology collects and examines biomaterials from patients with Alzheimer's, Parkinson's and other diseases to better understand the causes and courses of these conditions. Biomaterials include blood (e.g. DNA, RNA, serum, plasma, white blood cells, whole blood) and cerebrospinal fluid as well as urine and skin cells.
A central biobank guarantees the collection of high-quality biomaterials on a structured and standardized basis. What are the samples used for? For example, the examination of samples allows the quick investigation of the function and significance of a newly discovered gene, protein or other body substance. In this regard, a biobank is an important interconnection between basic research and medical care.
For materials from patients with neurodegenerative diseases, the biobank is run jointly be the Hertie Institute for Clinical Brain Research and the German Center for Neurodegenerative Diseases (DZNE).
The biobank materials are available to researchers with a focus on neurological diseases or neurosciences. Materials are also provided to third parties after careful project evaluation in order to support and facilitate scientific cooperations.
The biobank has been approved by the local ethics committee.
More information
A special biobank for neurological research
Article about the Biobank on the website Baden-Württemberg healthcare industry (25.06.2012)
Rückblick: Biovalley Meet&Match "Neurological and Psychiatric Disorders"
Article by BIOPRO Baden-Württemberg (13.12.2012) (in German only)
What is collected and how
The Biobank receives samples from donors who are patients at the Clinical Department of Neurology or participants in studies. When asked to donate samples to the biobank, you will receive detailed oral and written information about the process the samples are taken, stored and used. If you agree to donate, you will be asked to sign a consent form.
I want to donate biological samples to the biobank. What do I need to do?
If you want to donate samples to the biobank, please write an email neuro_biobank(at)hih-tuebingen.de or call us (07071 29 80472) to get more information.
Sample collection and data security
We can only gain knowledge from biomaterials if the samples are collected together with some personal information, such as age, sex, type and severity of a disease. These data are subject to the biobank secrecy and are stored in connection with a code number. This number is used in further investigations and statistical analysis ("pseudonymization"). People who work with your material do not know your name.
The biobank secrecy
- applies from the time point of sample collection for the duration of its continued existence,
- limits the processing and transfer of samples and related data to the purpose of scientific research only,
- guarantees the inaccessibility to people not involved in research projects,
- allows the intended use and restricted transfer of samples and data,
- applies to all persons involved in the collection and usage of biobank data,
- guarantees that no measures are taken to identify the donor,
- ensures that private entities (insurance companies, employers, etc.) do not get access to biobank data,
- guarantees that involved persons are bound to professional discretion
A sample transfer is always carried out using a code number. The number allows no conclusion to be drawn about the donor. Personal data will not be given to third parties.
Destruction of samples and data
There is no destruction of biological samples planned. However, you may withdraw your consent to the storage of your samples and data at any time. Following your cancellation, all samples stored in the biobank at the time will be destructed and corresponding personal data will be deleted (except disease-related data such as gender, age, or diagnosis). In this way we guarantee a complete anonymization of already used samples and do not compromise ongoing scientific investigations by data destruction. Existing research results will not be destroyed as long as the data is anonymized or already published (e.g. in case reports). Samples that have been given to cooperation partners will not destructed.
Reports on new findings
We do not use to inform donors on new findings. However, in case of relevant scientific questions and/or health-related findings, we may inform in individual donor. This is based on the written agreement of the donor to be contacted at a later date.
Selected Publications
2024
Roeben B, Liepelt-Scarfone I, Lerche S, Zimmermann M, Wurster I, Sunkel U, et al. Longitudinal cognitive decline characterizes the profile of non-PD-manifest GBA1 mutation carriers. NPJ Parkinsons Dis. 2024;10(1):88.
Zanon A, Guida M, Lavdas AA, Corti C, Castelo Rueda MP, Negro A, et al. Intracellular delivery of Parkin-RING0-based fragments corrects Parkin-induced mitochondrial dysfunction through interaction with SLP-2. J Transl Med. 2024;22(1):59.
Maass F, Canaslan S, van Riesen C, Hermann P, Schmitz M, Schulte C, et al. Myelin basic protein and TREM2 quantification in the CSF of patients with Multiple System Atrophy and other Parkinsonian conditions. J Neurol. 2024;272(1):52.
2023
Rattay TW, Volker M, Rautenberg M, Kessler C, Wurster I, Winter N, et al. The prodromal phase of hereditary spastic paraplegia type 4: the preSPG4 cohort study. Brain. 2023;146(3):1093-102.
Koros C, Brockmann K, Simitsi AM, Bougea A, Liu H, Hauser AK, et al. Impact of APOE Genotype on Cognition in Idiopathic and Genetic Forms of Parkinson's Disease. Mov Disord. 2023;38(5):907-9.
Lerche S, Zimmermann M, Roeben B, Wurster I, Fries FL, Deuschle C, et al. Inflammatory CSF profiles and longitudinal development of cognitive decline in sporadic and GBA-associated PD. NPJ Parkinsons Dis. 2023;9(1):38.
2022
Konstantin Nissen S, Farmen K, Carstensen M, Schulte C, Goldeck D, Brockmann K, et al. Changes in CD163+, CD11b+, and CCR2+ peripheral monocytes relate to Parkinson's disease and cognition. Brain Behav Immun. 2022;101:182-93.
Schmidt S, Luecken MD, Trumbach D, Hembach S, Niedermeier KM, Wenck N, et al. Primary cilia and SHH signaling impairments in human and mouse models of Parkinson's disease. Nat Commun. 2022;13(1):4819.
Kessler C, Ruschil C, Abdelhak A, Wilke C, Maleska A, Kuhle J, et al. Serum Neurofilament Light Chain and Glial Fibrillary Acidic Protein as Biomarkers in Primary Progressive Multiple Sclerosis and Hereditary Spastic Paraplegia Type 4. Int J Mol Sci. 2022;23(21).
2021
Becker S, Granert O, Timmers M, Pilotto A, Van Nueten L, Roeben B, et al. Association of Hippocampal Subfields, CSF Biomarkers, and Cognition in Patients With Parkinson Disease Without Dementia. Neurology. 2021;96(6):e904-e15.
Pilotto A, Zipser CM, Leks E, Haas D, Gramer G, Freisinger P, et al. Phenylalanine Effects on Brain Function in Adult Phenylketonuria. Neurology. 2021;96(3):e399-e411.
Heinzel S, Aho VTE, Suenkel U, von Thaler AK, Schulte C, Deuschle C, et al. Gut Microbiome Signatures of Risk and Prodromal Markers of Parkinson Disease. Ann Neurol. 2021;90(3):E1-E12.
2020
Wilke C, Haas E, Reetz K, Faber J, Garcia-Moreno H, Santana MM, et al. Neurofilaments in spinocerebellar ataxia type 3: blood biomarkers at the preataxic and ataxic stage in humans and mice. EMBO Mol Med. 2020;12(7):e11803.
Lerche S, Wurster I, Roeben B, Zimmermann M, Riebenbauer B, Deuschle C, et al. Parkinson's Disease: Glucocerebrosidase 1 Mutation Severity Is Associated with CSF Alpha-Synuclein Profiles. Mov Disord. 2020;35(3):495-9.
Wilke C, Dos Santos MCT, Schulte C, Deuschle C, Scheller D, Verbelen M, et al. Intraindividual Neurofilament Dynamics in Serum Mark the Conversion to Sporadic Parkinson's Disease. Mov Disord. 2020;35(7):1233-8.
2019
Lerche S, Machetanz G, Wurster I, Roeben B, Zimmermann M, Pilotto A, et al. Dementia with lewy bodies: GBA1 mutations are associated with cerebrospinal fluid alpha-synuclein profile. Mov Disord. 2019;34(7):1069-73.
Nissen SK, Shrivastava K, Schulte C, Otzen DE, Goldeck D, Berg D, et al. Alterations in Blood Monocyte Functions in Parkinson's Disease. Mov Disord. 2019;34(11):1711-21.
Lerche S, Wurster I, Roben B, Machetanz G, Zimmermann M, Bernhard F, et al. Parkinson's disease: evolution of cognitive impairment and CSF Abeta(1-42) profiles in a prospective longitudinal study. J Neurol Neurosurg Psychiatry. 2019;90(2):165-70.
2018
Blauwendraat C, Wilke C, Simon-Sanchez J, Jansen IE, Reifschneider A, Capell A, et al. The wide genetic landscape of clinical frontotemporal dementia: systematic combined sequencing of 121 consecutive subjects. Genet Med. 2018;20(2):240-9.
Lerche S, Liepelt-Scarfone I, Wurster I, Schulte C, Schaffer E, Roben B, et al. Polygenic load: Earlier disease onset but similar longitudinal progression in Parkinson's disease. Mov Disord. 2018;33(8):1349-53.
Wilke C, Rattay TW, Hengel H, Zimmermann M, Brockmann K, Schols L, et al. Serum neurofilament light chain is increased in hereditary spastic paraplegias. Ann Clin Transl Neurol. 2018;5(7):876-82.
2017
Lerche S, Schulte C, Srulijes K, Pilotto A, Rattay TW, Hauser AK, et al. Cognitive impairment in Glucocerebrosidase (GBA)-associated PD: Not primarily associated with cerebrospinal fluid Abeta and Tau profiles. Mov Disord. 2017;32(12):1780-3.
Brockmann K, Lerche S, Dilger SS, Stirnkorb JG, Apel A, Hauser AK, et al. SNPs in Abeta clearance proteins: Lower CSF Abeta1-42 levels and earlier onset of dementia in PD. Neurology. 2017;89(23):2335-40.
Wilke C, Gillardon F, Deuschle C, Hobert MA, Jansen IE, Metzger FG, et al. Cerebrospinal Fluid Progranulin, but Not Serum Progranulin, Is Reduced in GRN-Negative Frontotemporal Dementia. Neurodegener Dis. 2017;17(2-3):83-8.
2016
Bacioglu M, Maia LF, Preische O, Schelle J, Apel A, Kaeser SA, et al. Neurofilament Light Chain in Blood and CSF as Marker of Disease Progression in Mouse Models and in Neurodegenerative Diseases. Neuron. 2016;91(1):56-66.
Sailer A, Scholz SW, Nalls MA, Schulte C, Federoff M, Price TR, et al. A genome-wide association study in multiple system atrophy. Neurology. 2016;87(15):1591-8.
Wilke C, Preische O, Deuschle C, Roeben B, Apel A, Barro C, et al. Neurofilament light chain in FTD is elevated not only in cerebrospinal fluid, but also in serum. J Neurol Neurosurg Psychiatry. 2016;87(11):1270-2.
2015
Jansen IE, Bras JM, Lesage S, Schulte C, Gibbs JR, Nalls MA, et al. CHCHD2 and Parkinson's disease. Lancet Neurol. 2015;14(7):678-9.
Laske C, Stellos K, Kempter I, Stransky E, Maetzler W, Fleming I, et al. Increased cerebrospinal fluid calpain activity and microparticle levels in Alzheimer's disease. Alzheimers Dement. 2015;11(5):465-74.
Brockmann K, Srulijes K, Pflederer S, Hauser AK, Schulte C, Maetzler W, et al. GBA-associated Parkinson's disease: reduced survival and more rapid progression in a prospective longitudinal study. Mov Disord. 2015;30(3):407-11.
2014
Nalls MA, Pankratz N, Lill CM, Do CB, Hernandez DG, Saad M, et al. Large-scale meta-analysis of genome-wide association data identifies six new risk loci for Parkinson's disease. Nat Genet. 2014;46(9):989-93.
Vijayaraghavan S, Maetzler W, Reimold M, Lithner CU, Liepelt-Scarfone I, Berg D, et al. High apolipoprotein E in cerebrospinal fluid of patients with Lewy body disorders is associated with dementia. Alzheimers Dement. 2014;10(5):530-40 e1.
Schondorf DC, Aureli M, McAllister FE, Hindley CJ, Mayer F, Schmid B, et al. iPSC-derived neurons from GBA1-associated Parkinson's disease patients show autophagic defects and impaired calcium homeostasis. Nat Commun. 2014;5:4028.
2013
Reinhardt P, Schmid B, Burbulla LF, Schondorf DC, Wagner L, Glatza M, et al. Genetic correction of a LRRK2 mutation in human iPSCs links parkinsonian neurodegeneration to ERK-dependent changes in gene expression. Cell Stem Cell. 2013;12(3):354-67.
Holmans P, Moskvina V, Jones L, Sharma M, International Parkinson's Disease Genomics C, Vedernikov A, et al. A pathway-based analysis provides additional support for an immune-related genetic susceptibility to Parkinson's disease. Hum Mol Genet. 2013;22(5):1039-49.
Klebe S, Golmard JL, Nalls MA, Saad M, Singleton AB, Bras JM, et al. The Val158Met COMT polymorphism is a modifier of the age at onset in Parkinson's disease with a sexual dimorphism. J Neurol Neurosurg Psychiatry. 2013;84(6):666-73.
2012
Sathe K, Maetzler W, Lang JD, Mounsey RB, Fleckenstein C, Martin HL, et al. S100B is increased in Parkinson's disease and ablation protects against MPTP-induced toxicity through the RAGE and TNF-alpha pathway. Brain. 2012;135(Pt 11):3336-47.
Blauw HM, van Rheenen W, Koppers M, Van Damme P, Waibel S, Lemmens R, et al. NIPA1 polyalanine repeat expansions are associated with amyotrophic lateral sclerosis. Hum Mol Genet. 2012;21(11):2497-502.
Synofzik M, Maetzler W, Grehl T, Prudlo J, Vom Hagen JM, Haack T, et al. Screening in ALS and FTD patients reveals 3 novel UBQLN2 mutations outside the PXX domain and a pure FTD phenotype. Neurobiol Aging. 2012;33(12):2949 e13-7.
2011
International Parkinson Disease Genomics C, Nalls MA, Plagnol V, Hernandez DG, Sharma M, Sheerin UM, et al. Imputation of sequence variants for identification of genetic risks for Parkinson's disease: a meta-analysis of genome-wide association studies. Lancet. 2011;377(9766):641-9.
Hoglinger GU, Melhem NM, Dickson DW, Sleiman PM, Wang LS, Klei L, et al. Identification of common variants influencing risk of the tauopathy progressive supranuclear palsy. Nat Genet. 2011;43(7):699-705.
Ross OA, Soto-Ortolaza AI, Heckman MG, Aasly JO, Abahuni N, Annesi G, et al. Association of LRRK2 exonic variants with susceptibility to Parkinson's disease: a case-control study. Lancet Neurol. 2011;10(10):898-908.
2010
Blauw HM, Al-Chalabi A, Andersen PM, van Vught PW, Diekstra FP, van Es MA, et al. A large genome scan for rare CNVs in amyotrophic lateral sclerosis. Hum Mol Genet. 2010;19(20):4091-9.
Laske C, Stransky E, Hoffmann N, Maetzler W, Straten G, Eschweiler GW, et al. Macrophage colony-stimulating factor (M-CSF) in plasma and CSF of patients with mild cognitive impairment and Alzheimer's disease. Curr Alzheimer Res. 2010;7(5):409-14.
Synofzik M, Fernandez-Santiago R, Maetzler W, Schols L, Andersen PM. The human G93A SOD1 phenotype closely resembles sporadic amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry. 2010;81(7):764-7.
2009
Sidransky E, Nalls MA, Aasly JO, Aharon-Peretz J, Annesi G, Barbosa ER, et al. Multicenter analysis of glucocerebrosidase mutations in Parkinson's disease. N Engl J Med. 2009;361(17):1651-61.
Simon-Sanchez J, Schulte C, Bras JM, Sharma M, Gibbs JR, Berg D, et al. Genome-wide association study reveals genetic risk underlying Parkinson's disease. Nat Genet. 2009;41(12):1308-12.
Scholz SW, Houlden H, Schulte C, Sharma M, Li A, Berg D, et al. SNCA variants are associated with increased risk for multiple system atrophy. Ann Neurol. 2009;65(5):610-4.
The Neuro-Biobank Tübingen takes samples from donors with an existing comprehensive demographic and clinical dataset. Clinical diagnosis is made by experienced specialists in the field. Sample processing is fast and follows standardized operating procedures. Sample and data quality, as well as processing quality are regularly checked. Thus the biobank can offer biomaterial specimens of highest standards. The aim of our biobank is to offer principle investigators the opportunity to request samples for specific projects. Proposals will be reviewed by a steering committee, to decide on priorities.
Researchers interested in collaboration projects with the Biobank may contact neuro-biobank@medizin.uni-tuebingen.de for both informal and formal requests. Formal requests should include (see template):
- Type of material, number of samples and amount of material needed (in detail):
- Title of the Research Project
- Background and objective of the proposed project
- Own previous results relevant for the project
- Study outline
- Estimated start and end of the study (please insert dates)
- Authorized Signature of the Applicant
- Recipient's Official and Mailing Address, phone, fax, email
Coordinator: Prof. Dr. Kathrin Brockmann
Administrative coordinator: Claudia Schulte
Clinical organization: Ina Wolfstädter
Assistant medical technicians: Christian Deuschle (head), Ann-Kathrin-Hauser, Benjamin Riebenbauer
Data protection coordinator: Christian Erhardt
Steering committee: Prof. Dr. Thomas Gasser, Prof. Dr. Mathias Jucker, Prof. Dr. Holger Lerche, Prof. Dr. Ulf Ziemann

Claudia Schulte
Center of Neurology, Department of Neurodegenerative Diseases and Hertie Institute for Clinical Brain Research
University Hospital Tübingen
Otfried-Mueller-Str. 27
72076 Tübingen
claudia.schulte(at)uni-tuebingen.de







